Information for Patients & Carers
Regional Post Critical Care Support Group
A support group has been set up to help people and their families, who have previously spent time on critical care units within West Yorkshire and Harrogate
You are welcome to drop in and share your experiences with others, or to just listen.
Complimentary refreshments will be available.
Hospital staff based from the LTHT critical care units and critical care rehabilitation team will be present at the group to help answer and questions and provide information as required.
Social distancing and COVID safety measures will be in place.
Please feel free to drop in once or to attend regularly.
When: 5pm - 7pm every first Thursday of each month
Where: Thackray Medical Museum, Beckett Street, Leeds, LS9 7TF (Parking is available)
For further information: Email: [email protected] or call: 0113 206 8961
To download flyer click here >>>>>>>
A support group has been set up to help people and their families, who have previously spent time on critical care units within West Yorkshire and Harrogate
You are welcome to drop in and share your experiences with others, or to just listen.
Complimentary refreshments will be available.
Hospital staff based from the LTHT critical care units and critical care rehabilitation team will be present at the group to help answer and questions and provide information as required.
Social distancing and COVID safety measures will be in place.
Please feel free to drop in once or to attend regularly.
When: 5pm - 7pm every first Thursday of each month
Where: Thackray Medical Museum, Beckett Street, Leeds, LS9 7TF (Parking is available)
For further information: Email: [email protected] or call: 0113 206 8961
To download flyer click here >>>>>>>
Critical Care is a term now used for an area in the hospital, which provides two levels of care for patients, although in some hospitals this may be in two separate areas. These patients will be the sickest patients in the hospital from a severe illness or injury. The aim is to achieve the best possible recovery, although this is not always possible and because they are so ill, some patients will die in Critical Care. When recovery becomes impossible the focus of care changes to making the patient as comfortable as possible.
The information below is aimed at patients and relatives who are going through the critical care journey.
The information below is aimed at patients and relatives who are going through the critical care journey.
|
What is Critical Care
Critical Care is a term now used for an area in the hospital which provides two levels of care for patients, Intensive Care and High Dependency Care. In some hospitals both Intensive care and High Dependency patients are located in a single unit. In other hospitals the units will be separate. Generally patients admitted to Intensive Care will require specialist monitoring and equipment to take over the work of one or more of their body's organs such as breathing or the work of the kidneys. There is a nurse allocated to care for each patient 24 hours a day (1:1 nurse:patient). Patients cared for in High Dependency (HDU) require a level of care between intensive therapy and the general hospital wards. Examples would be patients who no longer need intensive therapy but need step-down care or patients admitted from wards, theatres or Emergency Departments who need more treatments than can be provided in a ward area. Although the equipment is often the same as in Intensive Care most patients need less specialist equipment and the nursing ratio is one nurse to every two patients, 24 hours a day (1:2 nurse:patients). What to expect
Visiting a loved one in critical care for the first time can be a frightening experience. It is normal to feel upset at seeing someone you love in Critical Care. Most patients in Critical Care will be connected to machines or drips of some sort. It is important for you to know that an alarm going off does not immediately translate to a problem or emergency. Many of the machines have alarms that sound to let staff know that something needs doing, for example if a drip needs to be changed. Usually, there is nothing to worry about the staff will closely watch the patient at all times. In the first few days following admission many patients are kept sedated with a mixture of sleep inducing and pain killing medications. Some of the life-saving treatments required in Critical Care are uncomfortable or unpleasant and the sedation makes this more bearable for the patient, as well as allowing them to rest. They might not remember this time, although sedated patients may be able hear you even if they do not respond. The staff will talk to unconscious patients telling them whats happening and we suggest you do the same. There may be times when staff will ask you to leave the patientʼs bedside. This is because some of the necessary medical procedures are not pleasant and may upset you. It also gives the staff room to do their job. As patients start to improve their sedation will be reduced to allow them to become more aware of their surroundings. It can be frightening to wake up in a strange place and it can take some time for the sedative drugs to wash out the patient’s system. They often find the presence of family and friends reassuring at this time. Some patients get better quickly and are soon ready to leave the Critical Care , for others this may take longer as they need support, particularly from the ventilator, or breathing machine, for some time. This slow recovery process is often called ‘weaning’ and although the patient is on the mend they can find this time very frustrating as their progress is slow, and they may not be able to talk, eat or drink. Mobilisation by the physiotherapy team at this time is vital in helping the patient regain the strength and co-ordination of their muscles. visiting
An ICU can often be an overwhelming place, both for the patient and their loved ones. It can therefore help to know a little about what to expect. Visiting hours are usually very flexible, but there may be times when visiting isn't advised so it's a good idea to check before you arrive. The number of people allowed around the person's bed may be limited. Sick patients need rest to help their recovery so it is advised that visitors should be kept to close family and friends. It is also suggested that a flow of visitors, spending long periods of time at the bedside may be exhausting for patients and should be avoided. At different intervals throughout the day it may be necessary to carry out essential nursing and sometimes, medical procedures. You may be asked to leave the unit for a short period of time, or until the task is completed. Occasionally, some nursing and medical procedures can take longer than anticipated. This may result in you being kept waiting to see your relative. We hope that you will appreciate that the care of your relative is of the utmost importance. Hygiene rules – to reduce the risk of spreading infection, you'll be asked to clean your hands when entering and leaving the unit and you may not be able to bring in certain things such as flowers. Avoid visiting if you're ill.. There is further information available in leaflet below. How patients may look and behave – the person you're visiting may be drowsy and seem confused. They may also appear slightly swollen or have injuries such as bruises or wounds. This can be upsetting to see, but staff will ensure they're as comfortable as possible. ICU equipment – a series of tubes, wires and cables will be attached to the patient, which may look alarming at first. Ask staff to explain what these are if you'd like to know. Unfamiliar sounds – you may hear alarms and bleeps from the equipment. These help staff to monitor their patients. You'll usually be free to touch, comfort and talk to the person. It may help them to hear and recognise familiar voices, even if they don't appear to respond. You might want to tell them about your day, or read them a book or newspaper. You can bring in things to make them more comfortable, but ask staff beforehand if there's anything you shouldn't bring. The ICU staff will be on hand during your visit to answer any questions you have.
Taking care of yourself This is probably a very stressful time in your life. People can have a range of reactions. You may feel anxious, tearful, angry, sad, guilty, frightened, shocked, a feeling of numbness or nothingness. People often talk of feeling helpless and frustrated, wishing that there were more they could do. All these reactions are NORMAL responses to having a relative as a patient within Critical Care. It is important that you take care of yourself. There is no right or wrong way of coping. Here are some ideas that people have found helpful:
Discharge to the ward
It is not unusual for both patients and relatives to feel anxious about moving from Critical Care to a ward area. You may have become familiar with the staff and routine on Critical Care. You may have felt reassured by the number of staff on Critical Care and monitoring equipment used to observe you. It is therefore important that you are prepared for your move and you feel reassured. The medical and nursing teams on the ward will get a thorough hand-over from the critical care team, and some hospitals have an outreach team consisting of ICU nurses who help patients, relatives and ward staff cope with the transition. The ICU team will try and prepare patients and families for ‘stepping down’ and viewing the more normal atmosphere of the general ward as an important step towards recovery and rehabilitation. Hospitals aim for transfers to happen in daytime, when more staff are available to help with settling in, although this is not always possible. Families will always be informed that the patient has moved so they come to the correct place at visiting time. Transfer back to the ward is a good thing as it means the patient no longer needs Critical Care, but the transition to the general ward environment can be challenging for both patient and family, particularly if the critical stay has been prolonged. Although critical care is difficult, it offers security that a patient’s every change is noticed, and need provided for. It is, however, not somewhere to stay if critical care is no longer required. On the ward, with less nursing and medical staff immediately to hand, patients and families can feel abandoned and anxious about a deterioration in the patient’s condition. This is normal and gets better in time as the patient continues to improve ICU Steps Information
The Intensive Care Unit Support Teams for Ex-Patients (ICUsteps) was founded in 2005 by ex-patients, their relatives and ICU staff to support patients and their families through the long road to recovery from critical illness. They have a very useful Patient Guide which contains advice and information about intensive care. It tells you how critical illness may be treated and what recovery may be like. Not every patient will experience all of these things, but they are more likely to if they have been in intensive care for more than a few days. Most of this guide is written for patients but there is a section specifically for relatives and visitors. By reading the guide, relatives will learn what a patient's recovery may involve and it will give them the answers to some of the questions they may have. Useful links for further information
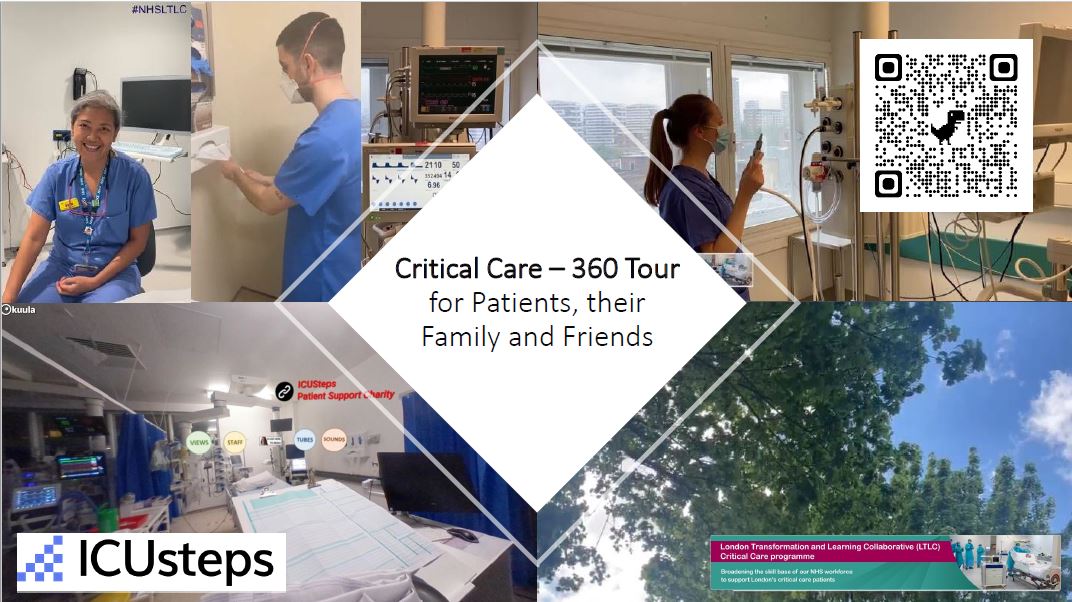
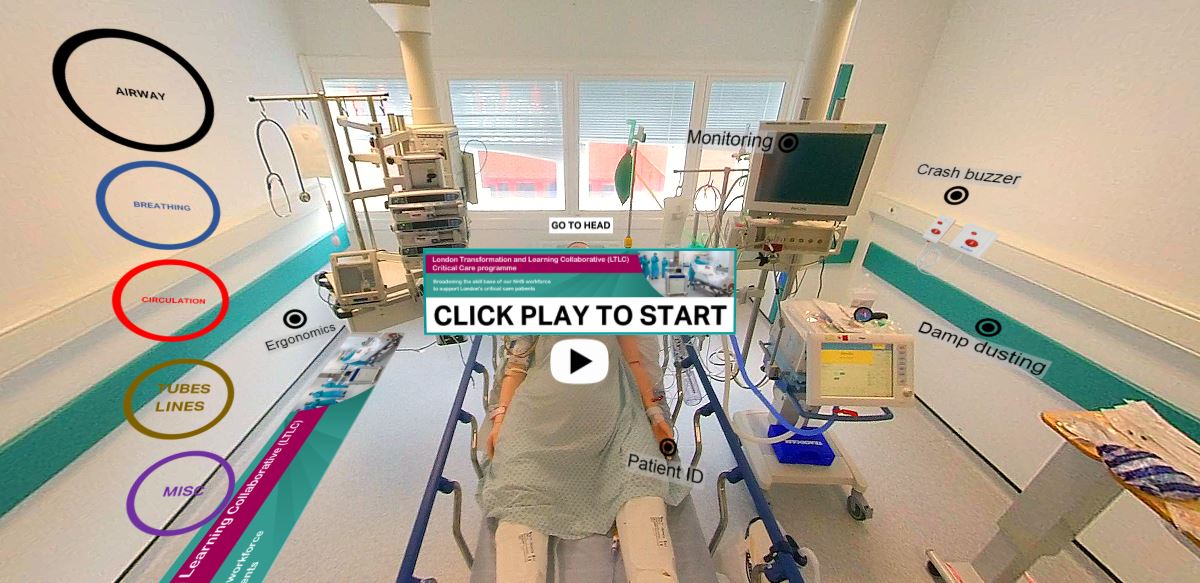
360 degree tour of Critical CareClick on the image below to take a 360 degree tour of Critical Care.
You can also take a look around a critical care bed space by clicking on the next image..
These resources have been developed by London Transformation and Learning Collaborative and ICU Steps with Patients, their family and friends in mind. Patient Experiences These are short videos of ex critical care patients sharing their experiences of their time spent on critical care. |
Healthcare staff are keen to prevent the spread of infection to patients whilst in hospital. This is even more important in critical car when patients are very sick and have less ability to fight bugs.
Please read the information in the guidance below so you can do your bit.
Information Leaflet for Visitors to Critical CareThis leaflet has been prepared to help guide you whilst visiting family and friends in the Critical Care Unit.
Exercise & Rehabilitation Booklet
This booklet has been developed by West Yorkshire Critical Care ODN Rehabilitation Forum. The exercises may help patients develop strength and fitness after critical illness. The exercises should be explained to the patient while in hospital, and are designed so that the patient can continue them at home. You should not exercise if you feel unwell. If you are unsure, please check with your GP, nurse or physiotherapist ICU Steps - Road to Recovery - Critical Care Rehabilitation Guide
This Rehabilitation Guide has been developed by a national working group of professionals working in Critical Care to provide patients with information to help support ongoing recovery after an admission to critical care. Bradford Teaching Hospitals have developed this online resource to support patients, their families and friends after they leave the intensive care unit. Although some aspects of this resource are directed at patients/family/friends who have been on the intensive care unit at Bradford, there is lots of information about how you can help yourself feel better and recover, and where you or your loved one can find support for both mental and physical health regardless of the intensive care unit you have stayed on. . | ||||||